ALBA Synchrotron
A team led by researchers from the Universitat Politècnica de Catalunya (UPC) has unveiled the mechanism of action of two drugs, FR60 and JNI18, which cure 100% of mice with sleeping sickness, also called African trypanosomiasis. Using synchrotron light at the ALBA Synchrotron, they have observed how these drugs perfectly stacked on the Trypanosoma brucei’s DNA, the parasite that causes the disease. Blocking and inflicting specific damage on its DNA, the parasite cannot reproduce and finally dies after 4-5 days. Scientists conclude drugs are effective potential treatments against sleeping sickness, which threats over 55 million people in sub-Saharan Africa countries. These drugs remain patent-free to gain interest among pharmaceutical labs.
Cerdanyola del Vallès, 16/11/2017.
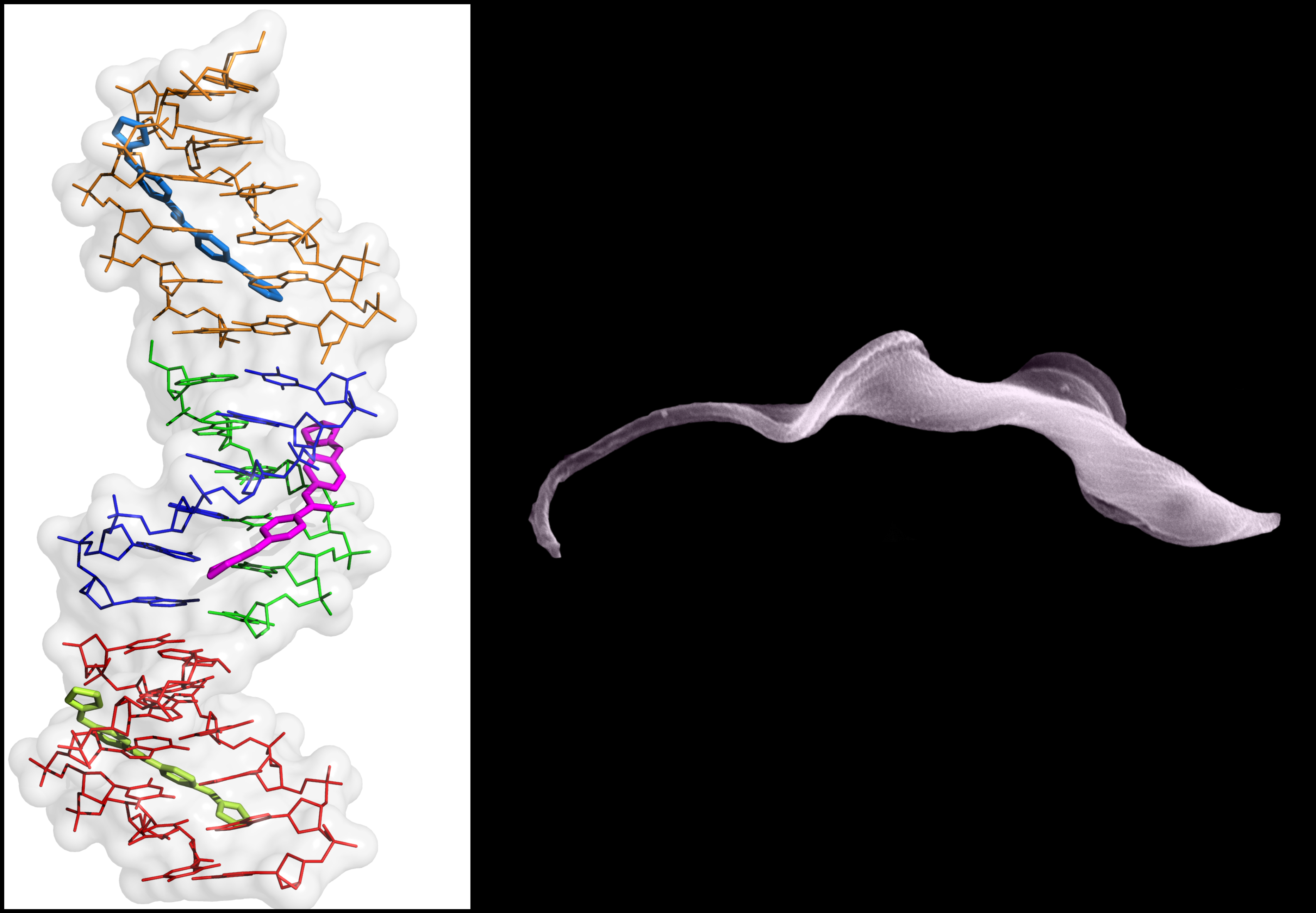
The main objective of this research – performed by scientists from UPC, the Spanish National Research Council (CSIC) and the University of Glasgow – was to prove the effectiveness of two new chemical compounds (FR60 and JNI18) to fight against the parasite Trypanosoma brucei, the responsible of African trypanosomiasis or sleeping sickness. Researchers also pursued to unveil the mechanism of action of these compounds to help in the design of new trypanocidal drugs. After carrying out different analysis and techniques, among which X-ray diffraction at the ALBA Synchrotron (which enables to solve molecules’ structures), scientists have demonstrated how these compounds block a Trypanosoma’s exclusive kind of DNA: the kinetoplast. The key finding is that drugs are bonded to the DNA helix, so its interaction with essential proteins for DNA maintenance is disrupted. "We observe the two drugs can displace these essential proteins from kinetoplast DNA (replace them) and alter DNA and parasite normal functions" explains Lourdes Campos, responsible of the Crystallography, Structure and Function of Biological Macromolecules (MACROM) group from UPC. 24 hours after the drug has been linked to DNA, the kinetoplast is extremely affected being disintegrated. Therefore, the parasite cannot reproduce and dies after 4-5 days. In conclusion, both drugs have been proved to be effectiveto fight against sleeping sickness, both the chronic and severe types and the veterinary form of the illness that affects cattle in Africa and causes serious economic problems.

Left: 3D structure obtained at XALOC beamline. It can be observed the kinetoplast DNA with 3 drug molecules perfectly linked (in blue, pink and phosphorescent green). Right: Trypanosoma brucei parasite (photo: Dr. Leandro Lemgruber).
A long casting to find the best drug
This study is a result of a collaborative work between international research centres. First, the Institute of Medical Chemistry (IQM-CSIC) designed and synthetized the new candidate drugs. The University of Glasgow, the College of Medical, Veterinary and Life Sciences - the Wellcome Centre for Molecular Parasitology, carried out the in vitro culture assays: they tested the parasite survival against the drugs, in order to select those most effective killing the parasite. Finally, the UPC MACROM group was able to obtain crystals of the drug-DNA complexes with the two chosen compounds: DNA-FR60 and DNA-JNI18. The crystals were analyzed at ALBA Synchrotron in XALOC beamline. Using X-ray diffraction, researchers could solve the 3D structure of all these complexes. This technique offers a great level of resolution, enabling to determine the interaction between drugs and DNA at atomic scale. The final results have been deposited in the public Protein Data Bank and confirmed that the target for both drugs is the kinetoplast DNA: it is clearly observed how the drugs cover the minor groove of DNA. These results and the other tests performed in Glasgow and at the Swiss Tropical and Public Health Institute (STPH) led us to state "both drugs are 100% curative in mice affected by African trypanosomiasis" concludes Lourdes Campos.
The research article published in Nucleic Acid Research – with a high impact factor in its field – has been selected as a highlight by the Spanish Biophysics Society
.
African trypanosomiasis or sleeping sickness: a neglected tropical disease
Like many other tropical illnesses, sleeping sickness is not under the focus of the pharmacy industry. The bite of an infected tsetse fly introduces the parasite inside the blood of the victim and, if the infection remains untreated, the ending is usually fatal. Nowadays, sleeping sickness threats over 55 million people distributed in 36 sub-Saharan African countries. Most of the affected population lives in remote areas in Africa’s poorest countries, with limited access to health services, which complicates the diagnosis and treatment of cases. Current drugs are extremely toxic and sometimes ineffective since resistance strains are frequent. For all these reasons, finding new safe and efficient drugs is urgently needed. FR60 and JNI18 drugs have not been patented to promote their study by all the interested laboratories and, if they are approved by the European Medicines Agency in the future, to distribute them easily at low-cost among the needy people.
It is not the first time Lourdes Campos' group, IQM-CSIC and the University of Glasgow investigate together a tropical disease. Three years ago, they already proved the effectiveness of a drug (CD27) against malaria with the same technique in ALBA Synchrotron. In fact, FR60 and JNI18 are derivatives from this malaria drug. Indeed, without knowing CD27 structure, FR60 and JNI18 could have not been synthetized. In Dr. Campos words "we investigate neglected disease precisely for this reason, because there are no many studies about them. Pharmaceutical companies don’t pay attention to this kind of illnesses because they are not lucrative, thinking as a company. So, academic laboratories must get involved to find new treatments. There is still a lot of work to do in this field".
Reference: Functional and structural analysis of AT-specific minor groove binders that disrupt DNA–protein interactions and cause disintegration of the Trypanosoma brucei kinetoplast (2017). Cinthia R. Millan Francisco J. Acosta-Reyes Laura Lagartera Godwin U. Ebiloma Leandro Lemgruber J. Jonathan Nué Martínez Núria Saperas Christophe Dardonville Harry P. de Koning J. Lourdes Campos. Nucleic Acids Research, Volume 45, Issue 14, Pages 8378–8391.